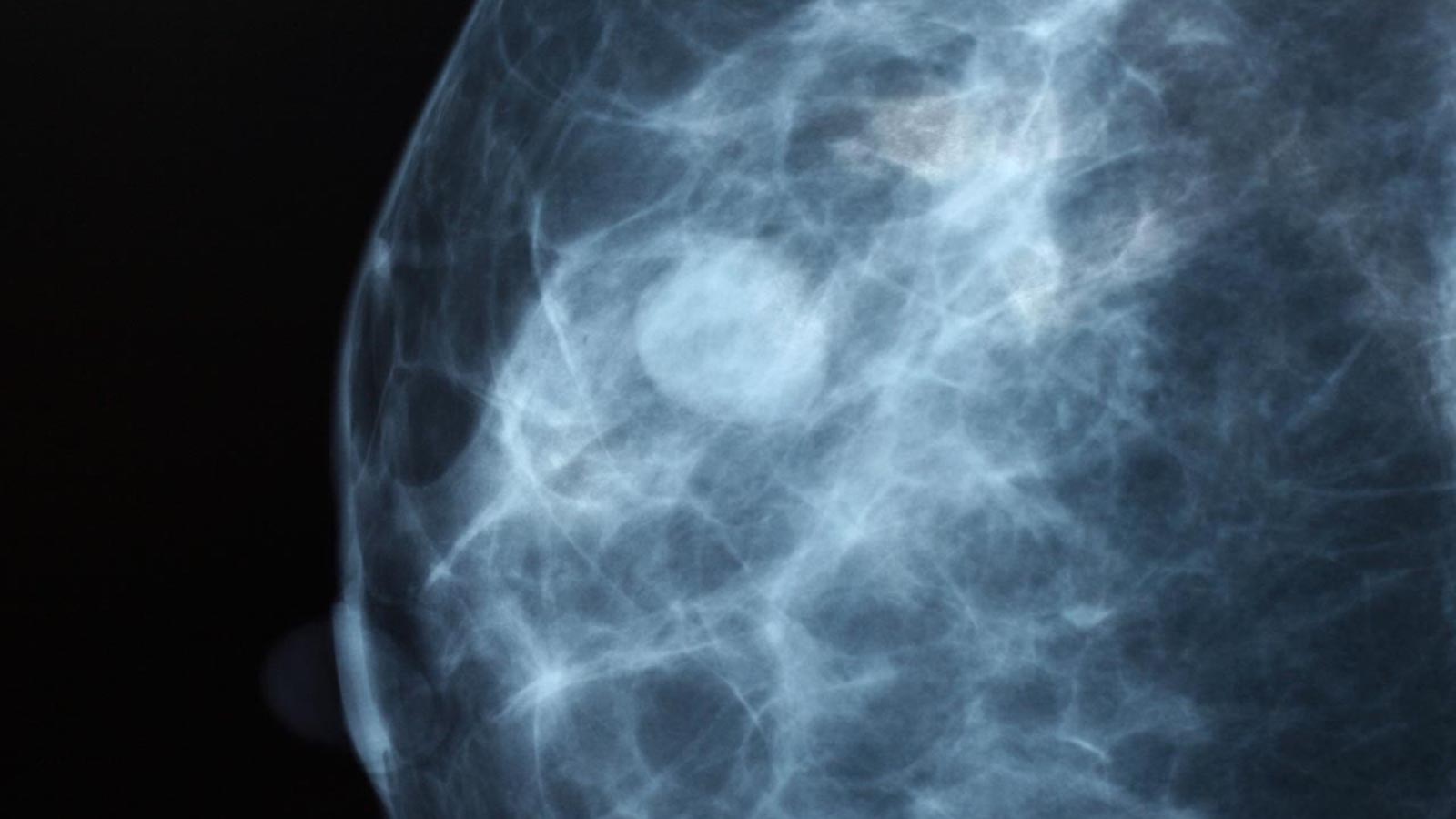
North Texas breast cancer patients in a clinical trial at UT Southwestern are receiving some of the most accurate imaging in the world to see if their tumors are responding to treatment, according to a new report from NBC 5.
Patients’ tumors are imaged with microbubbles and ultrasound devices that show great detail. Doctors can measure the tumors’ oxygenation and tissue pressure to determine how well chemotherapy works, even after a single treatment cycle.
Generally, a patient has to wait up to 12 or more cycles of chemotherapy, over six to eight months, to determine how well the treatment worked.
Doctors say this technology will help in early detection if the treatment is not working and save the patient months of toxic and high-cost treatment that is of no benefit.
“This is fast, simple, and also provides lots of functional information. That’s why I find it very groundbreaking,” said Dr. Basak Dogan, UT Southwestern professor and director of Breast Imaging Research.
Another benefit is that Optoacoustic imaging doesn’t use contrast or radiation, eliminating patient discomfort associated with MRI or CT.
Sue Henry of Waxahachie was a trial participant.
Henry got to see these images throughout her treatment and says seeing her tumor response to chemotherapy after each session gave her hope, according to NBC 5.
Her surgery to remove the remaining tumor after months of chemotherapy proved the imaging was accurate.
“It helped me wrap my brain around everything that was happening to me and that I was going to be OK,” said Henry.
Researchers are wrapping up their trial and will publish the results, says NBC 5.
“It’s very exciting for me because now we are actually questioning in these first group of patients who respond very, very well, whether they need surgery at all. So, I’m hoping that if we are good enough with this imaging technique, then we can tell the patients that their tumors are gone, and we don’t have to wait until they have surgery. They can choose to not have surgery,” said Dogan.