Shares of Biogen and other drugmakers researching Alzheimer’s disease soared early Wednesday after Japan’s Eisai Co.’s new drug to treat Alzheimer’s disease showed promise in a recent clinical trial.
The findings from a Phase 3 clinical trial have yet to be peer-reviewed in any medical journal. But according to a company news release, the drug lecanemab, compared with the placebo at 18 months, “reduced clinical decline on the global cognitive and functional scale” by 27%.
Eisai announced the results late Tuesday from a global study of nearly 1,800 people with early-stage Alzheimer’s whose progress was tracked over 18 months. Patients were monitored using a scale that measures mental decline and their ability to do daily activities like getting dressed or feeding themselves.
Eisai said it would discuss the full results of the research in late November “at the Clinical Trials on Alzheimer’s Congress (CTAD), and publish the findings in a peer-reviewed medical journal.”
The company is already seeking accelerated approval from the U.S. Food and Drug Administration, with a decision expected early next year. Eisai and Biogen will co-promote the drug.
In a statement, officials at the Alzheimer’s Discovery Drug Foundation (ADDF) said the study showed only “modest effectiveness” but stated this was still a good sign.
“The combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s,” said Dr. Howard Fillit, the co-founder and chief science officer at the ADDF.
“However, amyloid-clearing drugs will provide an incremental benefit at best and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging. We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting non-amyloid pathways of neurodegeneration.”
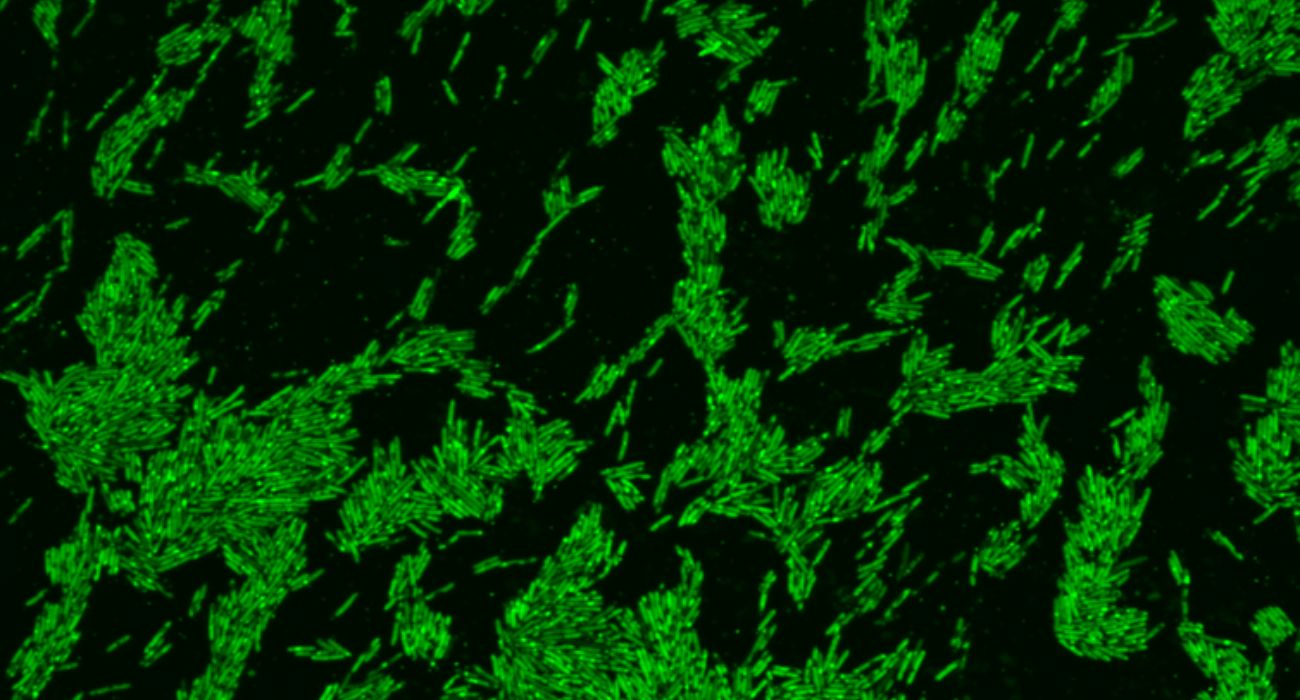
In earlier clinical trials, lecanemab was shown to lower levels of beta-amyloid plaque, a hallmark of the disease found in the brain of patients. Lecanemab is a monoclonal antibody drug designed to target and help remove Alzheimer’s-associated amyloid plaques in the brain in people with early Alzheimer’s.
“We know that it clears the beta-amyloid plaque,” said Dr. Scott A. Kaiser, a geriatrician and the director of geriatric cognitive health for the Pacific Neuroscience Institute at Providence Saint John’s Health Center in Santa Monica, California.
“The question is whether or not that actually helps with brain function,” Kaiser continued. “But the idea is that these plaques are interfering with the effective communication and overall interaction between brain cells and that clearing them could have positive effects.”
PET scans of the brains of patients who took lecanemab also showed noticeable declines in levels of the amyloid protein plaques.
As to possible side effects, there was an increase in cerebral hemorrhages known as “amyloid-related imaging abnormalities” (ARIA) in users of the drug, with 21.3% of patients on lecanemab presenting with the issue compared to 9.3% of those who took the placebo.
Some scientists have expressed concern with flaws in the earlier Phase 2 trials of lecanemab, suggesting that the actual benefit of the drug to people could be limited.
“The phase 2B lecanemab studies were fatally flawed because the high dose versus placebo analysis (that supposedly showed some clinical benefit) was profoundly compromised,” Dr. Michael Greicius, a professor of neurology and neurological sciences at Stanford University in California, told Healthline.
Greicius alleged that in the Phase 2B trial, people who were carriers of APOE4, a type of gene associated with an increased risk of Alzheimer’s disease, were prevented midway through the trial from receiving a high dose of the treatment.
“This means that there were many more APOE4 carriers in the placebo group (71 percent) than in the high dose group (30 percent),” Greicius explained. “This difference in percentage of APOE4 carriers is as likely (or in my view more likely) than the drug to account for the difference in clinical outcomes.”
It is estimated that nearly 6 million people in the United States are living with Alzheimer’s. The disease is a form of dementia that can progress from mild memory loss in the early stages to the potential for a person with the condition to have difficulty engaging in conversation or responding appropriately to what is around them.
There is currently no cure for Alzheimer’s, and treatment options are limited.